
How Long does Food Poisoning Really Last?
The Link Between Food Poisoning, IBS & SIBO
Most of us have had at least one unfortunate run-in with food poisoning: a bad taco, undercooked chicken, or a questionable potato salad sitting out at a barbecue that leaves us curled up in bed for 24 hours, swearing off leftovers. Usually, you recover and move on.
But what if that “stomach bug” never fully left?

Continuing research, led by Dr. Mark Pimentel, renowned gastroenterologist and executive director of the Medically Associated Science and Technology (MAST) Program at Cedars-Sinai, is changing how we think about foodborne illness. For some, a single episode of food poisoning can set off a domino effect in the gut, causing long-term disruptions that evolve into Irritable Bowel Syndrome (IBS), Small Intestinal Bacterial Overgrowth (SIBO), or both. If you've been struggling with bloating, abdominal pain, constipation, or diarrhea for months or years, there's a real chance it started with something you ate.
The good news? Understanding this post-infectious process opens the door to better testing, clearer answers, and more effective treatment.
A Hidden Epidemic: How Common is Food Poisoning, Really?
The Centers for Disease Control and Prevention (CDC) estimates that 48 million Americans get sick from foodborne illnesses each year, which translates to about 1 in 6 people. This is an astounding figure! Yet most cases go undiagnosed. Many people never even realize they had food poisoning, and only a small fraction of those who experience acute bouts of these types of symptoms ever get tested or are able to definitively identify the root cause.
The most common culprits–Campylobacter, Salmonella, E. coli, and Shigella–often cause fever, vomiting, diarrhea, and cramping. In most people, the immune system kicks in relatively quickly and resolves the issue in a few days or less. But for others, it’s not that simple.

Studies are now indicating that 10-20% of people who experience a foodborne illness go on to develop post-infectious IBS, making it the leading known cause of IBS around the world. For them, the initial symptoms fade, but their gut never quite returns to normal. Months later, they start noticing frequent bloating, irregular bowel movements, abdominal pain, or other debilitating gastrointestinal symptoms that often affect their daily routine and quality of life. But by then, the food poisoning is a distant memory, if they remember it at all.
To complicate matters, food poisoning cases are up to 10x more likely in the summer months. From July through September, heat and humidity help bacteria thrive in foods left too long in warm environments. Outdoor eating, travel, and more relaxed food safety habits make summer the prime time for gut trouble.
The Science: How Bacteria Can Break Your Gut
So how exactly does food poisoning turn into something chronic, or even life-changing?
According to Dr. Pimentel, the answer lies in an autoimmune reaction triggered by Cytolethal Distending Toxin B or CdtB, a toxin released by bacteria linked to food poisoning. When your body identifies that CdtB is present, your immune system goes to work, fighting back with an antibody aimed at eliminating the toxin. This antibody is aptly named anti-CdtB. This is a typical type of immune response, and your body is doing what it is designed to do, which is generally a good thing!
Unfortunately, CdtB also looks in some ways like something called vinculin, a naturally occurring protein in your body that helps to regulate gut motility (keeping food in your gut moving in a regular fashion) and is critical for healthy gut function. And because CdtB and vinculin look alike, your body may mistakenly think it also needs to fight back against vinculin too. So, it produces another antibody called anti-vinculin.

This phenomenon, known as molecular mimicry, causes collateral damage to the gut’s interstitial cells of Cajal–the cells that help your intestines contract and move food through your system. As these cells get damaged, gut motility slows. Bacteria that–under normal circumstances would be flushed downstream in regular cleansing cycles–stall out and begin to accumulate in the small intestine. This sets the stage for bacterial overgrowths like SIBO, IMO, and ISO which can cause bloating, gas, diarrhea, constipation, and many other symptoms that affect both your bathroom habits and quality of life.
Notably, these symptoms can appear weeks, months, or even years after the original infection. By then, most people have forgotten about the food poisoning episode entirely. They may chalk up their gut issues to stress, gluten, age, or just “sensitive digestion.” But what they’re experiencing is a cascade of changes initiated by a very specific bacterial encounter.
Diagnosing the Root Cause
Until recently, IBS was often labeled a “diagnosis of exclusion.” That means doctors would rule out everything else (like Crohn’s disease, celiac, or colon cancer) then hand over the IBS label. But now, thanks to new science, there are tools that can pinpoint the exact cause of many IBS and SIBO cases.
IBS-Smart: Testing for Post-Infectious IBS
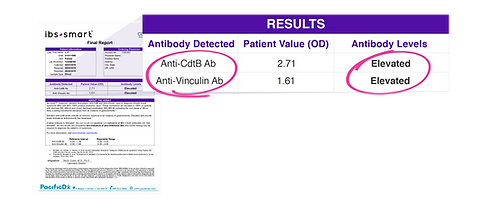
The IBS-Smart test, developed by Gemelli Biotech, measures the exact antibodies identified in post-infectious IBS patients: anti-CdtB and anti-vinculin. If these antibodies are both elevated, it’s a strong signal that your IBS symptoms stem from a prior foodborne illness. In fact, research now shows that the correlation is so strong that patients whose results show sufficiently elevated numbers of both antibodies have a 98% chance of being diagnosed with IBS.

Trio-Smart: Breath Testing for Bacterial Overgrowth
While not as well-known to the general public as IBS, Small Intestinal Bacterial Overgrowth (SIBO), Intestinal Methanogen Overgrowth (IMO), and Intestinal Sulfide Overproduction (ISO) affect millions of people worldwide, and are also strongly linked to patients with IBS and IBS-like symptoms. To investigate the presence and severity of a potential bacterial overgrowth in your system, the Trio-Smart 3-Gas Breath Test measures three gases: hydrogen, methane, and hydrogen sulfide, which are produced by different types of microbial overgrowths in your gut. Measurements of each of these gases can provide valuable clues about what’s going on inside you.
Identifying if an overgrowth is present and which gases are elevated in your gut can help you find the most appropriate diagnosis for your condition and determine the most effective course of action, whether that’s rifaximin, neomycin, prokinetics, dietary strategies, or a combination of various therapies.
Why is testing so important?
Without proper testing, it can be a real struggle to determine what’s actually causing your issues. With a lack of information and appropriate medical guidance, many people suffer from a prolonged period of guesswork and ineffective symptom management. Sometimes that brings you short-term relief, but as Dr. Pimentel points out, “When you treat the symptoms, the underlying disease is still there.” And some of your behaviors or attempts at symptom management may even make your condition worse.

But when you start to get answers and explanations for what you’re going through, you get a renewed sense of relief and hope. As one patient told Cedars-Sinai after receiving her IBS diagnosis, “It was the first time I felt validated. I wasn’t crazy. There was a test that told me something was wrong. It wasn’t in my head. It wasn’t just stress.”
How to Know If This Could Be You
Many people with Post-Infectious IBS don’t remember the original infection—or never knew they had one. So how do you know if any of this applies to you?
Here are some common clues:
-
Your symptoms started suddenly, not gradually
-
Your symptoms began after travel, food poisoning, or a stomach virus
-
You had fever, vomiting, or diarrhea before symptoms started
-
You are experiencing chronic bloating, gas, diarrhea, or constipation
-
Your symptoms never fully resolve despite diet or lifestyle changes
-
You’ve been diagnosed with IBS but no one has mentioned a cause or tested you for PI-IBS or bacterial overgrowth
If any of this sounds familiar, you’re not alone. There are millions of potential new Post-Infectious IBS cases occurring each year, just in the United States. But the good news is, it’s possible to find real answers that help you treat or manage your condition.
Prevention and Protection
Of course, the absolute best way to deal with Post-Infectious IBS is to never get food poisoning in the first place. Here are a few steps to lower your risk:
-
Refrigerate leftovers quickly (usually within 2 hours, 1 hour if it’s hot outside)
-
Avoid cross-contamination: keep raw meat separate from cooked meat and produce
-
Wash your hands thoroughly before eating or preparing food
-
Be cautious when traveling–especially with street food or raw items
-
Use a food thermometer to ensure meats are cooked fully, adhering to USDA guidelines
-
Be extra vigilant during summer cookouts when food sits out too long
Once you've had food poisoning, your gut may be more vulnerable to ongoing or recurring issues. For people already diagnosed with Post-Infectious IBS or SIBO, flare-ups can happen more easily, even from mild exposures. Staying proactive with food safety helps protect your progress and will hopefully prevent any associated symptoms from getting worse.
A New Era of Answers
If you’ve been living with chronic GI issues like bloating, gas, pain, and unpredictable bowel habits, it’s time to ask: Could it all have started with a simple case of food poisoning?
For millions of people, the answer is yes.
Thanks to emerging research and new testing methods that have become both convenient and widely available, we now have the ability to see the fingerprints of past infection and help you find treatment and management options that are specifically tailored to your condition. Don’t give up! Keep researching, testing, and seeking expert medical advice until you find the answers–and the relief–that you deserve.
FAQ
Can food poisoning really lead to chronic illness?
Yes. In some people, the immune response to bacterial toxins damages the nerves in the gut, leading to chronic conditions like IBS and SIBO.
What is Post-Infectious IBS?
It’s a subtype of IBS that starts after a foodborne infection or stomach virus. It’s caused by antibodies that mistakenly attack gut nerve cells.
What do these at-home tests look for?
The IBS-Smart test checks for antibodies from food poisoning. The Trio-Smart 3-Gas Breath Test measures gases associated with bacterial overgrowth.
Where can I find out more about treatment for SIBO, IMO & ISO?
We’ve put together a comprehensive guide about these conditions, from testing to treatment. You can read it here: https://www.triosmartbreath.com/treatments
References:
https://www.cdc.gov/food-safety/about/index.html
https://www.foodsafety.gov/food-poisoning/bacteria-and-viruses
https://www.gastrojournal.org/article/S0016-5085(17)30008-2/fulltext
https://www.health.com/foodborne-illness-summer-increase-safety-11763963
https://drruscio.com/new-ibs-test/
https://www.youtube.com/watch?v=TMTB9yfaskY
https://www.cedars-sinai.org/blog/causes-and-treatments-for-irritable-bowel-syndrome.html
https://www.cedars-sinai.org/blog/taking-back-control-from-ibs.html
